
Our Pipeline
Acellular Tissue Engineered Vessels
Acellular Tissue Engineered Vessels are tissue structures designed to resemble the body’s natural vasculature and aim to restore, replace, or enhance the function of damaged or diseased vascular tissue.
Our product candidates are currently in various stages of preclinical and human clinical studies to test the safety, efficacy, and viability of a first-of-its-kind investigational Acellular Tissue Engineered Vessel (ATEVTM) platform across a breadth of potential uses including Arteriovenous Access in Hemodialysis, Peripheral Artery Disease (PAD), Coronary Artery Bypass Grafting (CABG), and Pediatric Heart Surgery.
Stats from Acellular Tissue Engineered Vessel Clinical Trials and Expanded Access Patients
across multiple clinical applications
In order to administer dialysis, a long-standing point of access to the patient’s blood system is needed. It is through this point of access that blood is transferred between the patient and the dialysis machine. The current standard of care involves connecting the patient’s artery with a vein, known as an arteriovenous fistula or AV fistula (AVF). Humacyte’s investigational ATEV is designed to provide an alternative to current standards of care for hemodialysis patients with End-Stage Renal Disease (ESRD).
- Infection is the leading cause of morbidity and mortality in hemodialysis patients. This treatment puts patients at higher risk for serious infections because it requires frequent access to the bloodstream using needles.2
- Central venous catheters, which are long, thin tubes placed into a large vein for access to the bloodstream, carry the highest risk of infection for hemodialysis access, but patients may require them while Arterial Venous Fistulas (AVFs) are unusable.2
- AVFs can take weeks or months to mature and become usable for hemodialysis. Some AVFs may never mature, or may fail over time, all of which may result in longer catheter use while establishing a new access site.3,4
- Some patients can lack adequate veins to create an AVF and require other access options.5
annually1
Humacyte completed two Phase 2 studies and two Phase 3 trials to evaluate the ATEV in AV Access; including studies comparing to autologous arteriovenous fistula or ePTFE graft in patients with ESRD. An additional Phase 3 trial is ongoing.
*Results published in Journal of Vascular Surgery – Vascular Science
press release
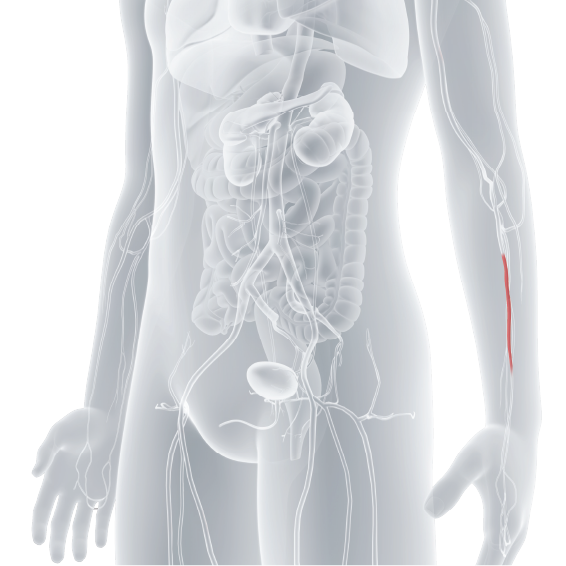
Peripheral artery disease (PAD) is a condition in which narrowed arteries restrict blood flow to a person’s arms or legs. PAD may cause pain, tissue damage, open sores, gangrene, and amputation.6 The ATEV platform is being investigated for use in PAD for arterial bypass procedures to determine its potential as a long-term option to restore blood flow to the affected limb and ultimately reduce the risk of amputation.
- When saphenous vein is not available, use of alternative conduits may be associated with risks of complications, such as infection, blood clots, and others.8
- The standard of care requires a second surgical site to harvest a saphenous vein to restore blood flow. However, approximately 40% of patients do not have a suitable saphenous vein available.9
have a suitable
saphenous vein available.9
Humacyte completed two Phase 2 human trials for the evaluation of the safety and efficacy of the 6mm ATEV in patients with peripheral artery disease (PAD).
*Results published in Journal of Vascular Surgery – Vascular Science
press release Read
press release
Coronary artery bypass surgery, also known as CABG, is a procedure to improve blood flow to the heart. Diseased arteries can limit oxygen reaching the heart muscle. In CABG, surgeons create detours around the blockages using healthy blood vessels from elsewhere in the body. This improves blood flow and can relieve chest pain and lower the risk of heart attack.
Using the patient’s veins is the standard in this procedure10 but, some patients may not have an available or suitable saphenous vein, for bypass procedures. Humacyte’s ATEV platform is being investigated as an alternative conduit for coronary artery bypass grafting (CABG).
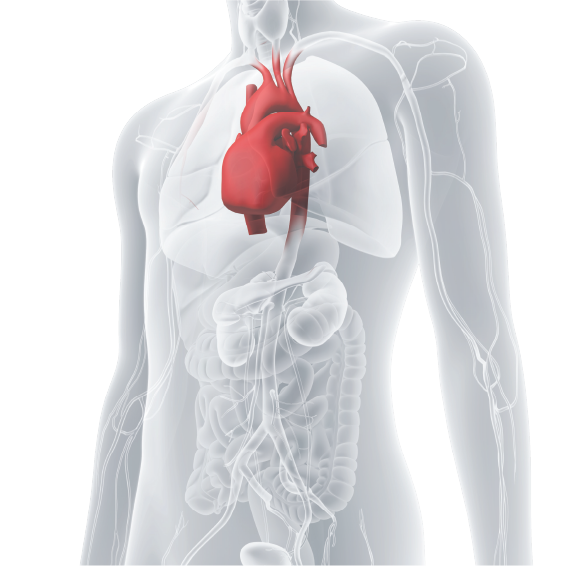
- In some cases, more than one vessel is needed to create multiple bypasses. This occurs when there are multiple blocked coronary arteries that require revascularization.11 Often the targeted donor vessels are unavailable or diseased, thereby providing a less than desired outcome.
- When suitable veins are available, surgeons perform a surgical harvesting procedure to obtain them. However, this procedure carries potential risks, including pain and complications associated with surgery.12
- Even if the harvested veins are successfully implanted, they don’t always remain open or patent. Over time, they may become narrowed or blocked again. As a result, some patients require a second procedure to restore blood flow and additional vein may need to be harvested or may not be available.13
Saphenous vein grafts may not be a durable solution for all patients:
Second surgical sites to harvest vein can be painful and complicated:
The Humacyte Coronary Artery Bypass Grafting (CABG) Program is currently in preclinical studies to evaluate safety and potential benefits of the smaller diameter 3.5mm ATEVs.
press release
Congenital heart defects (CHD) are associated with lifelong challenges, health services needs, and may require repeat surgical interventions. The Humacyte Pediatric Heart Surgery program is investigating the potential benefits of a smaller 3.5mm diameter ATEV in patients born with congenital heart defects.
Many babies are born each year with congenital heart disease and will face lifelong challenges. Unfortunately, many will undergo several reoperations as their bodies grow as some treatment options may not grow with the patient.
defects result in
Our research is focused on Tetralogy of Fallot, a heart condition that affects one in every 2,000 babies born each year and aims to assess the ATEV platform as a conduit to help repair the heart defect.15 The Humacyte Pediatric Heart Surgery Program is currently in preclinical studies to evaluate the safety and efficacy of the smaller 3.5mm diameter ATEVs in patients born with congenital heart defects.
press release
- National ESRD Census Data. esrdnetworks.org. Accessed December 30, 2023. https://esrdnetworks.org/resources-news/national-esrd-census-data/.
- Rha B, See I, Dunham L, et al. Vital Signs: Health Disparities in Hemodialysis-Associated Staphylococcus aureus Bloodstream Infections — United States, 2017–2020. MMWR Morb Mortal Wkly Rep 2023;72:153–159.
- Allon M, Robbin ML. Increasing arteriovenous fistulas in hemodialysis patients: Problems and solutions. Kidney International. 2002;62(4):1109-1124. doi:10.1111/j.1523-1755.2002.kid551.x.
- Schinstock CA, Albright RC, Williams AW, et al. Outcomes of arteriovenous fistula creation after the Fistula First Initiative. Clin J Am Soc Nephrol. 2011;6(8):1996-2002. doi:10.2215/CJN.11251210.
- Al-Jaishi AA, Oliver MJ, Thomas SM, Lok CE, Zhang JC, Garg AX, Kosa SD, Quinn RR, Moist LM, Patency Rates of the Arteriovenous Fistula for Hemodialysis: A Systematic Review and Metaanalysis. American Journal of Kidney Diseases 63, 464–478 (2014).
- Peripheral Artery Disease - Living With | NHLBI, NIH. www.nhlbi.nih.gov. https://www.nhlbi.nih.gov/health/peripheral-artery-disease/living-with.
- Peripheral Artery Disease National Action Plan. www.heart.org. November 21, 2023. Accessed December 12, 2024. https://www.heart.org/en/health-topics/peripheral-artery-disease/pad-resources/pad-action-plan.
- Kinlay S. Management of Critical Limb Ischemia. Circ Cardiovasc Interv. 2016 Feb;9(2):e001946.
- Taylor LM, Edwards JM, Brant B, Phinney ES, Porter JM. Autogenous reversed vein bypass for lower extremity ischemia in patients with absent or inadequate greater saphenous vein. The American Journal of Surgery. 1987;153(5):505-510. doi:https://doi.org/10.1016/0002-9610(87)90803-8.
- Caliskan E, de Souza DR, B.ning A, et al. Saphenous vein grafts in contemporary coronary artery bypass graft surgery. Nature Reviews Cardiology. 2019;17(3):155-169. doi:https://doi.org/10.1038/s41569-019-0249-3.
- Cleveland Clinic. Coronary Artery Bypass Surgery | Cleveland Clinic. Cleveland Clinic. Published 2018. https://my.clevelandclinic.org/health/treatments/16897-coronary-artery-bypass-surgery.
- Garland R, et al. A retrospective audit of long-term lower limb complications following leg vein harvesting for coronary artery bypass grafting. Eur J Cardiothorac Surg. 2003 Jun;23(6):950-5. doi: 10.1016/s1010-7940(03)00116-7. PMID: 12829071.
- Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GDavid, Burton JR. Coronary bypass graft fate and patient outcome: Angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. Journal of the American College of Cardiology. 1996;28(3):616-626. doi:https://doi.org/10.1016/0735-1097(96)00206-9.
- Gilboa SM, Devine OJ, Kucik JE, et al. Congenital Heart Defects in the United States. Circulation. 2016;134(2):101-109. doi:https://doi.org/10.1161/circulationaha.115.019307.
- Stallings EB, Isenburg JL, Rutkowski RE, et al. National population-based estimates for major birth defects, 2016-2020. Birth Defects Research. 2024;116(1):e2301. doi:https://doi.org/10.1002/bdr2.2301.
